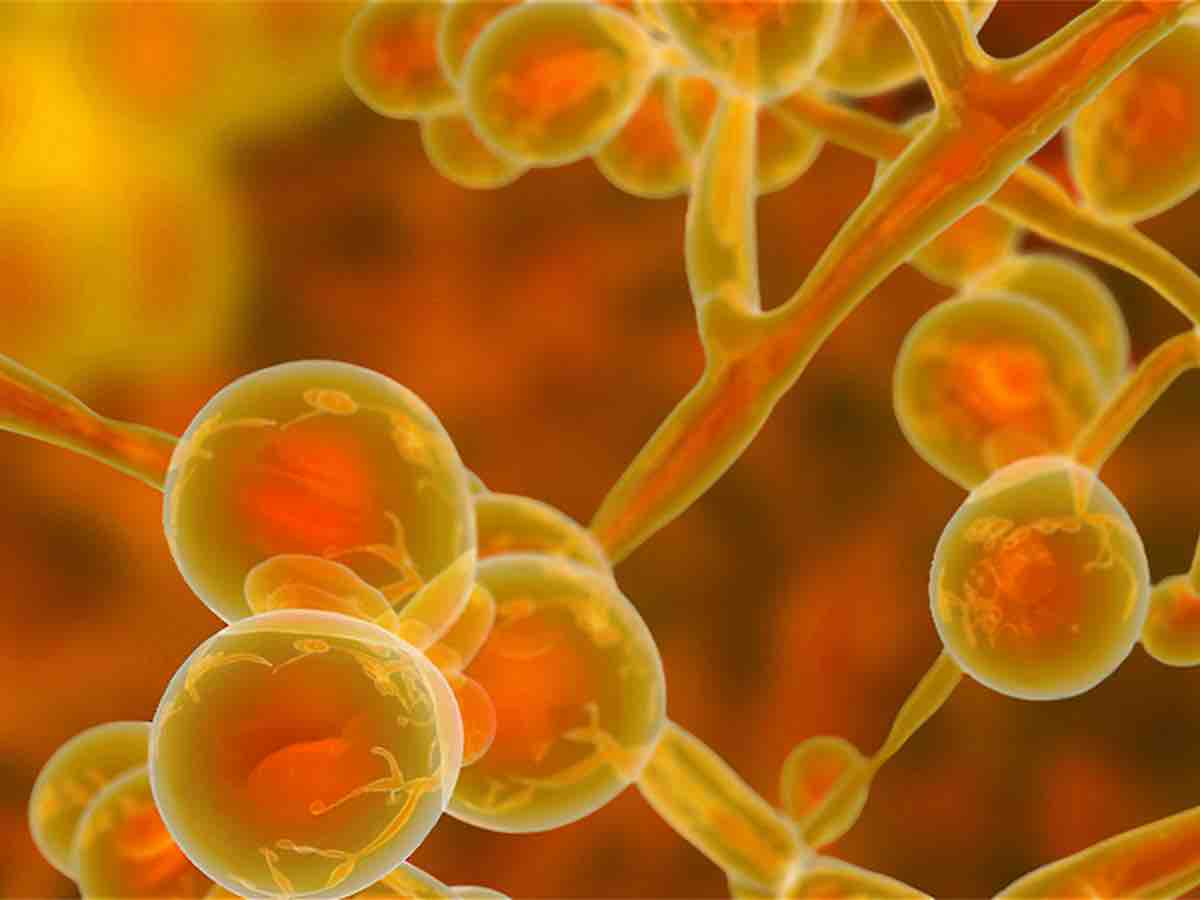
The fungal pathogen Candida auris has become a significant global health concern, posing a severe ecological security threat worldwide. As a result of its rapid and widespread emergence, almost certainly driven by climate change and ecological disruption, this highly virulent multi-compound resistant superbug has caused severe infections, high mortality rates, and persistent outbreaks. Moreover, because of its expanding resistance to existing antifungal treatments and ecological and socioeconomic impacts, Candida auris will almost certainly have long-lasting ramifications for human insecurity and political instability.
Origins of Candida Auris
Scientists identified the first isolate of Candida auris in a Japanese patient’s ear canal in 2009. The second isolation was reported in 2011 from a patient’s external ear canal discharge in South Korea, leading to a recognition that the pathogen was expanding geographically. However, retrospective reviews of fungal strain libraries found that Candida auris had been collected by at least 1996 in South Korea. Since then, it has rapidly spread across the globe, causing severe infections and outbreaks in more than 30 countries.
The pathogen’s origin remains a mystery. The widespread use of antifungal drugs may have contributed to Candida auris’ emergence, but it does not explain why the fungus became pathogenic simultaneously on three continents (Asia, Africa, and South America). As resistance and virulence are distinct properties, it is unlikely the acquisition of compound resistance played the sole role. Instead, the evidence suggests that transcontinental factors may have influenced the emergence of virulence in Candida auris.
Candida Auris and the Climate Change Hypothesis
Scientists have recently proposed climate change as a critical facilitator of the fungus’s adaptation to higher temperatures—and, indeed, global warming is a transcontinental stressor. The hypothesis argues that Candida auris and other fungi exposed to warming conditions experience a selection pressure to evolve greater thermotolerance. This step is essential for fungal pathogenicity since the higher internal temperatures in mammals make them far less susceptible to fungal diseases than other animals.
But this hypothesis would suffer without evidence that Candida auris existed in the environment before its recent isolation. After all, thermotolerance is unlikely to have evolved within temperature-regulated organisms such as humans, irrespective of rising outdoor temperatures. Moreover, discovering environmental samples of Candida auris would imply these fungi could withstand significant variations of biophysical stress, conferring a hardiness unlikely to be found in those that evolved to adapt to specific conditions within humans. Environmental conditions also expose fungi to ecological stresses, such as predation by amoeba and other microorganisms, that tend to select for virulence traits.
That evidence came in 2021 when a team of Indian scientists reported that Candida auris had been isolated from samples from the coastal wetlands of the Andaman Islands, which is 850 miles east of the Indian subcontinent. The fungus was isolated from two sites—a salt marsh and a sandy beach—in virgin habitats around the island group far removed from human activity. Furthermore, the same study revealed wild Candida auris had considerable intrinsic resistance to high temperatures, suggesting a relatively small jump in heat tolerance was required to reach mammalian temperatures.

An additional aspect of the question of Candida auris’ origin bears mention. As discussed in the SIPRI report Five Urgent Questions on Ecological Security, scientists and policymakers have a persistent—and, frankly, maddening—tendency to frame antimicrobial resistance (AMR) solely due to poor or inappropriate use of antimicrobial drugs. If the ecological dimensions of AMR are overlooked, it is impossible to comprehend the effects of climate change and other elements of ecological disruption on AMR. Moreover, when practitioners use terms like “drug resistance” instead of “antimicrobial resistance”, they further undermine the clear ecological dimensions of AMR.
Candida auris Health Effects
Candida auris is a formidable fungal pathogen that poses significant health risks due to its multidrug-resistant nature and its ability to cause severe infections, particularly in individuals with weakened immune systems. Patients undergoing chemotherapy, organ transplants, or suffering from chronic diseases are more susceptible to infections, which can target blood vessels, urinary tracts, surgical and open wounds, and the ear.
The fungal pathogen can survive on surfaces for weeks or even months in healthcare settings. As a result, Candida auris can persist on bed rails, chairs, floors, and medical equipment, despite routine cleaning and disinfection, leading to unexpected outbreaks that can be difficult to contain. As with other fungal pathogens, some infections can become chronic, persisting for long periods and requiring prolonged treatment (which increases the risk of emerging antifungal resistance).
The similarities between fungal and human cells make it challenging to develop synthetic antifungal drugs that target fungi without harming human cells. Hence, far fewer antifungal drugs are available than antibiotics for bacterial infections. Consequently, fungal pathogens that develop resistance to multiple drugs/compounds are especially worrying. In 2021, the Centers for Disease Control and Prevention (CDC) announced that some Candida auris strains are now resistant to all known classes of antifungal compounds.
Candida auris Effects on Livestock and Other Animals
Limited information is available on the effects of Candida auris on other mammals, including livestock, since most studies and reports focus on human health. However, it is worth noting that other Candida species have been associated with infections in animals, including livestock. For example, the pathogen has been found to cause mastitis in dairy cattle, a mammary gland inflammation that can lead to decreased milk production and quality. Candidiasis is a disease that afflicts dogs, cats, horses, and nonmammals such as birds, reptiles, amphibians, and fish.
Security implications of Candida auris
Candida auris seriously threatens global economies and political stability, especially if it continues to escape antifungal treatments. The pathogen could overwhelm healthcare systems, significantly straining government resources. Due to the rapid spread of this deadly fungus, economic growth could be stifled, and income inequality is likely to worsen. Furthermore, the inability to contain and treat infections could undermine public trust in political leaders and healthcare systems, potentially contributing to social and political unrest.
The emergence and intensification of Candida auris emphasize the importance of conceptualizing such ecological threats as security threats. International cooperation and investments in public health infrastructure will be needed to mitigate the effects of this emerging global threat on economies and politics worldwide.